Elizabeth Fuemmeler, AuD, and Daniel Romero, AuD, discussed dizziness and the importance of seeing an audiologist. If you are experiencing dizziness or balance problems, find an audiologist in your area and schedule a screening today.
What Is Dizziness?
Dizziness is a term people use to describe a variety of sensations. Symptoms such as vertigo, disequilibrium, lightheadedness, and spatial disorientation can all be described as dizziness. However, each symptom and their description offer unique insight into the problem as well as the possible cause.
On average 1 in 4 people would experience some form of dizziness in their lives. However, dizziness can mean different things to different people. It can be described as a…
- spinning sensation (true vertigo)
- lightheadedness
- general imbalance/unsteadiness
- [spatial] disorientation
- motion intolerance (Teggi, 2016)
The frequency, duration, and intensity of these symptoms can also vary. For some, they can be transient, and for others chronic. Dizziness may affect the young and the older population indiscriminately. It can manifest as delayed developmental milestones, general clumsiness in children; loss of confidence within athletes; and increased fall risks in older adults.
Regardless, being dizzy can be a jarring experience. all, being able to maintain one’s balance is critical to survival; it correlates with fall risks; increased level of fear/anxiety; and impacts the ability to remain independent.
When seeking help for your dizziness, it is imperative to include an audiological consult. The ear plays a significant role in maintaining equilibrium. There are structures within the ear dedicated to the detection of spinning movement (i.e., angular acceleration) and gravity (i.e., linear acceleration). When the ears are impacted, it confuses the brain’s ability to find a reference point and maintain steadiness.
Some common causes of dizziness episodes can be inflammation of the inner ear structures, changes in inner ear status, decline(s) in the cognitive system, and deterioration of the cardiovascular system.
Audiologists are typically trained to tease or rule out probable causes of your dizziness. Through hearing and balance diagnostic evaluations, an audiological consult can better dictate treatment plans and improve outcomes.
What Causes Hearing Loss and Balance Problems?
Before treating your dizziness, it is important to determine the cause of your dizziness. It is often best to contact your family physician and describe your symptoms to him or her. Your description may include how long the symptoms last, as well as movements, positions, situations, or times that seem to cause the symptoms to start, or to make them worse.
Pay attention to new or associated symptoms that occur around the same time as the dizziness such as headache, ringing in the ear(s), changes in hearing, pressure in the ears, or increased sensitivity to light or sound.
Dizziness can be caused by a variety of issues.
- Inner ear infections
- Meniere’s Disease
- Head injury
- Medications toxic to the ear
- Tumors
- Genetics
- Blood circulation
Rarely, dizziness is a medical emergency. If you experience slurred speech, confusion, difficulty swallowing, or the inability to walk, dial 911 or see a physician immediately.
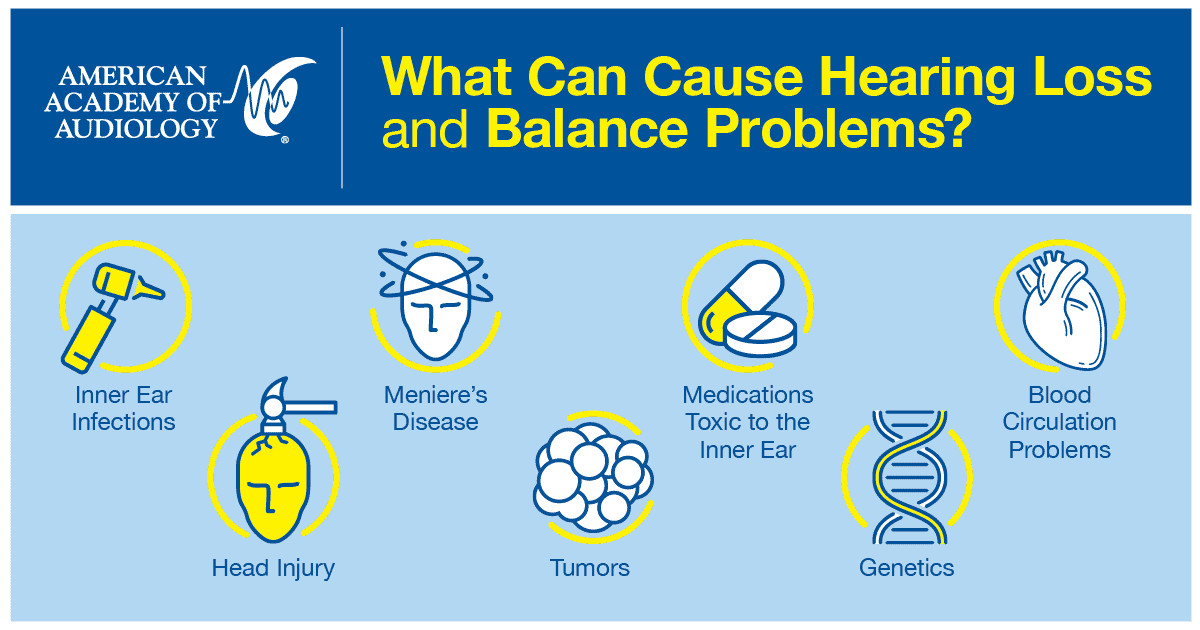
Gain a clearer understanding of the topic through our informative infographics.
Does Hearing Loss Affect Balance?
The inner ear is responsible for both hearing and balance function. Hearing loss indicates that there is a problem with the hearing organ (cochlea) in the inner ear. Problems with the inner ear may also include the balance organs due to an underlying condition that impacts the inner ear as a whole.
Change in Hearing and Balance Often Happen as We Age
Individuals with untreated hearing loss are more likely to have a history of falling (Lin, 2012; Vilkanen, 2009). They may also have
- Reduced vestibular and balance system function.
- Reduced awareness of the surroundings.
- Reduced cognitive resources available for balance due to hearing loss.
Improve Your Balance
Rummalla et al (2014) suggests the following to help improve your balance:
- Consider conditions such as vision changes and reduced sensitivity in your feet.
- Ask your health-care provider about the impact of your medications on dizziness and balance concerns.
- According to the National Institute on Aging, you should have your hearing tested annually. If you have concerns about your balance or hearing, evaluation by an audiologist can help identify the cause.
- Ask your health-care team about balance therapy options that can improve your balance.
- Evaluate your home for risks.
- Remove tripping hazards such as rugs.
- Use non-slip mats in the shower or bath.
- Add handrails in the bathtub and next to the toilet.
References
Lin FR, Ferrucci L. (2012) Hearing loss and falls among older adults in the United States. Arch Intern Med 172(4):369–371.
National Institute on Aging. Prevent Falls and Fractures [online]. www.nia.nih.gov/health/prevent-falls-and-fractures. Accessed July 3, 2019.
Rummalla K, Karin AM, Hullar TE. (2014) The effect of hearing aids on postural stability. Laryngoscope 125(3):720–723.
Teggi R et al. (2016) Point prevalence of vertigo and dizziness in a sample of 2,672 subjects and correlation with headaches. Acta otorhinolaryngologica 36(3):215–219. https://doi.org/10.14639/0392-100X-847.
Vilkanen A, Kaprio J, Pyykkö I, et al. (2009) Hearing as a predictor of falls and postural balance in older female twins. J Gerontol Biol Sci Med Sci 64(2):312–317.