Coding and Reimbursement Overview
The American Academy of Audiology (the Academy) has an active role in establishing and/or revising Current Procedural Terminology (CPT®) codes for new/existing procedures relevant to the practice of audiology. The Academy has official Advisors to the American Medical Association’s (AMA) CPT process for the creation and revision of codes. In addition to the establishment of new codes, the Academy engages in the AMA Relative Value Scale (RVS) Update Committee (RUC) process for valuation of codes.
Once a category I CPT code is created, the Academy is involved in surveying the work and practice expense of the procedure, and present the findings to the RUC. The RUC’s recommendations are submitted to the Centers for Medicare and Medicaid Services (CMS), who makes the ultimate assignment of reimbursement values for the procedure under the Medicare Physician Fee Schedule (MPFS).
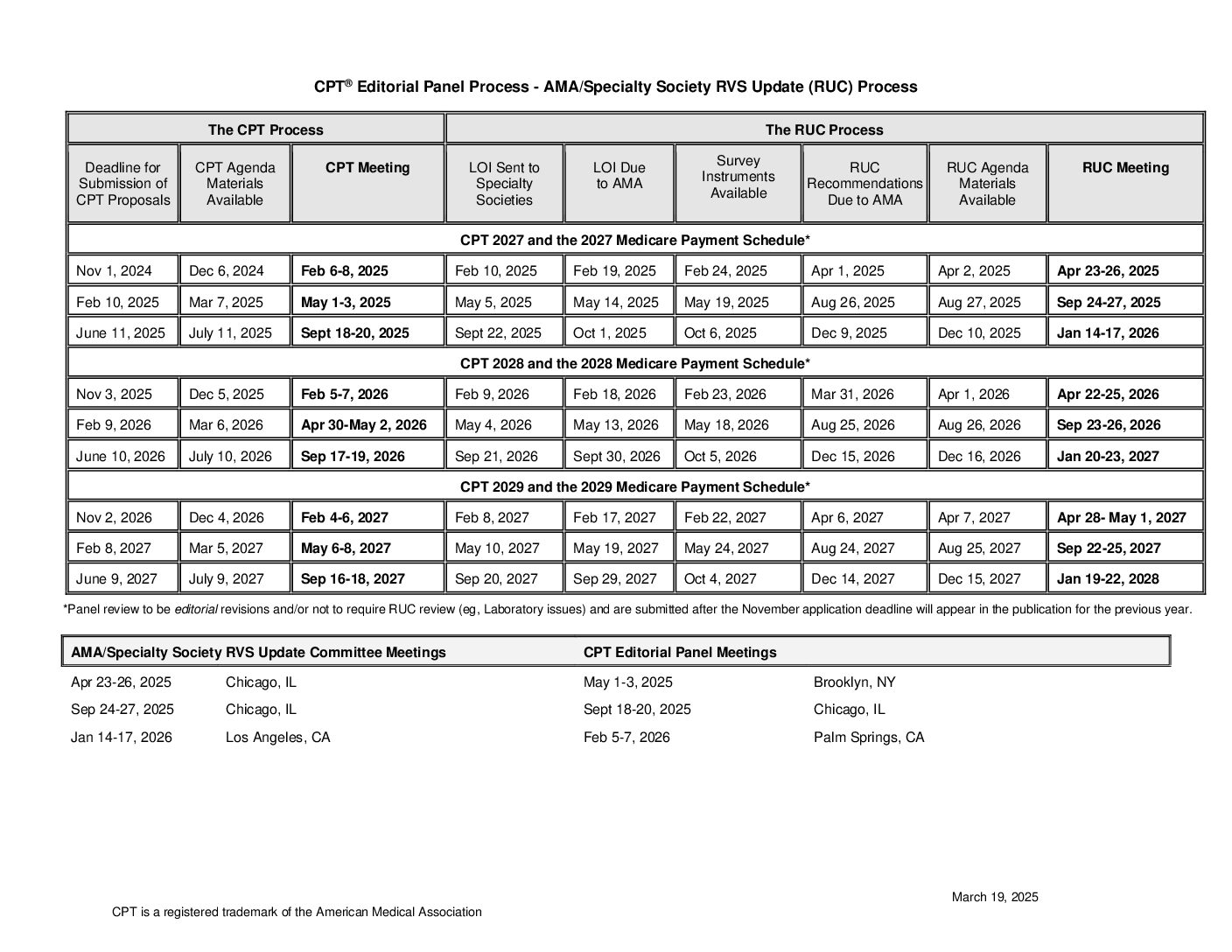
A full copy of the calendar and additional information from AMA can be found here.
Guidance to Industry and Individuals on Creating and Revising CPT Codes
If you are seeking to revise or create codes, please refer to the Academy’s “Guidance to Industry and Individuals on Creating and Revising CPT Codes.” The document includes a description of the AMA’s criteria for codes, followed by a series of questions to guide the development of a specific code proposal.
Coding Resources
This section provides coding information and resources, such as billing templates, guidance on modifier usage, Medically Unlikely Edits and the National Correct Coding Initiative, to make sure that you correctly follow current procedures. You will also find answers to your most Frequently Asked Coding-Related Questions. An additional resource for addressing coding questions is the regular column in Audiology Today. A compilation of the coding articles from 2017-2021 is available for reference.
Have additional coding, reimbursement, or compliance questions? E-mail the Academy’s reimbursement mailbox. By submitting questions to the centralized mailbox, the Academy’s Coding and Reimbursement Committee (CRC) is able to review and discuss all inquiries posed to the Academy. This allows the CRC to research responses, identify trends in coding and reimbursement, develop coding and reimbursement resources, and engage in advocacy with payers regarding policies.
01/01/2021 (revised 04/06/2021)
ICD-10 Codes
The Academy’s Coding and Reimbursement Committee (CRC) has developed a list of ICD-10 coding information and resources for audiologists to use in their audiology practice.
CMS Proposes 2025 Payment Rules
On July 10, 2024, the Centers for Medicare and Medicaid Services (CMS) released the proposed calendar year (CY) 2025 Medicare Physician Fee Schedule (MPFS) and CY 2025 Hospital Outpatient Prospective Payment System (OPPS) rules. Once final, the rules would take effect January 1, 2025.
New Audiology CPT Codes Introduced in 2021
The American Academy of Audiology (Academy) and the American Speech-Language-Hearing Association (ASHA) are pleased to announce the publication of seven new Current Procedural Terminology (CPT ®) codes for auditory-evoked potentials (AEP) and vestibular-evoked myogenic potential (VEMP) services. The American Medical Association (AMA) CPT Editorial Panel approved these codes for implementation on January 1, 2021.
CMS Expands List of Medicare Eligible Telehealth Providers to Include Audiologists
On April 30, 2020, the Centers for Medicare and Medicaid Services (CMS) issued an interim final regulation that states that all professionals who are able to bill Medicare for their professional services will be considered eligible telehealth providers for the duration of the COVID-19 public health emergency. Though not named specifically in the CMS Fact Sheet or Press Release, it is our interpretation of the regulation that audiologists are considered eligible providers of telehealth services.
RUC Survey Information
The AMA/Specialty Society RVS Update Committee conducts surveys to help with recommending accurate relative values for physician/clinician work to the Centers for Medicare and Medicaid Services (CMS). Surveys are comprised of questions relative to the physician/clinician work for one or more services. Individuals who receive a survey should complete and return it as an important contribution to their profession. Watch a video provided by the AMA to understand better the survey purpose and how to complete it.